HIV: 40 years of pandemic
- After infection with HIV, AIDS develops in three stages: the primary infection; the asymptomatic phase; and the lethal weakening of the immune system.
- Since the beginning of the pandemic in the 1980s, 40 million people have died, about as many as are currently living with the virus.
- HIV is a deadly retrovirus, but antiretroviral treatments exist to keep it under control, including tri-therapy.
- Pre-exposure prophylaxis consists of taking a combination of antiretroviral drugs prior to risky situations and can drastically reduce the risk of infection.
- Approximately 1.5 million people worldwide were infected with HIV in 2021 and 650,000 died from AIDS.
The thirtieth edition of the CROI (Conference on Retroviruses and Opportunistic Infections)1, which brings together specialists in Human Immunodeficiency Virus (HIV), was held last February. Let’s take it as an opportunity to take stock of the current situation of HIV in the world!
This virus was identified and isolated in 1983 by a team from the Pasteur Institute2. Like other scientists at the time, they were looking for the origin of a weakening of the immune system, observed in a growing number of patients in the United States since 1981 – the infamous acquired immunodeficiency syndrome (or AIDS). HIV has the particularity of infecting cells of the immune system, in particular T lymphocytes carrying the CD4 marker, often called T4 lymphocytes. These cells are progressively killed by the virus and their disappearance eventually prevents the body from defending itself against other infections. There are different types of HIV, derived from several adaptations of monkey viruses to humans. The one at the origin of the current pandemic, HIV‑1 type M, is thought to have emerged in the 1920s in Kinshasa3.
From HIV to AIDS
HIV can be transmitted through three bodily fluids: blood, sexual secretions, and breast milk. The development of AIDS following infection takes place in three stages. During the primary infection, i.e. the encounter with the virus, it multiplies in the body and the CD4 cell count drops. Anti-HIV antibodies begin to be produced and will remain detectable in the blood of patients, who thus become HIV-positive. As such, the term “HIV-positive” means “having antibodies” and is sometimes used without specifying the infectious agent involved when referring to HIV.
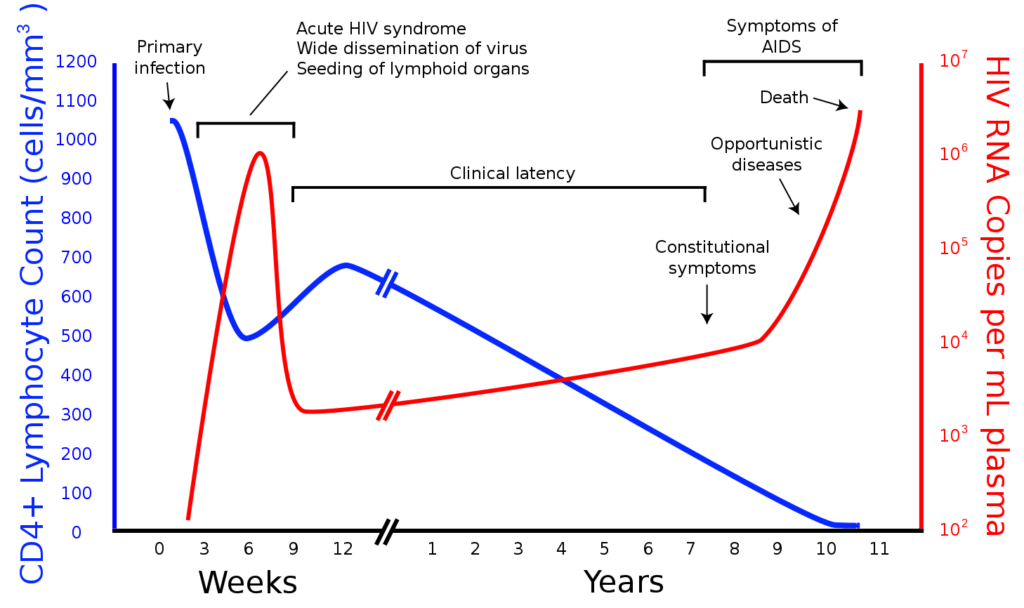
The immune system takes over after a few weeks, keeping the virus under control during an asymptomatic phase that can last up to ten years. This represents a first difficulty in the fight against HIV. Indeed, these patients who have no symptoms and often do not know that they are infected can still be contagious. It is both to enable treatment to be put in place and to avoid involuntary contamination during this asymptomatic phase that screening is essential.
After a while, HIV weakens the immune system enough to multiply again in the body. This is when AIDS begins: the body can no longer effectively defend itself against opportunistic infections which, if left untreated, will eventually lead to death.
Fighting HIV
HIV is a deadly retrovirus, but fortunately there are treatments that can keep it under control. Antiretroviral medications generally combine molecules targeting three different stages of the virus’ multiplication cycle, hence the term “tri-therapy”. This combination of several active ingredients is essential to control HIV because the virus mutates a lot, allowing it to develop resistance. The more we restrain it, the lower the probability that it will succeed in adapting.
The different components of tri-therapy can now be combined in a single tablet to be taken daily. They block the growth of the virus to the point where it is undetectable in the body, which has two enormous advantages. On the one hand, as the immune system is no longer under attack, it can once again play its protective role and prevent the development of AIDS. Moreover, the earlier the treatment is taken, the less the immune system has suffered beforehand and the more effective it is. If a risk is identified, it is possible to take emergency post-exposure treatment within 48 hours to try to prevent the virus from taking hold. In addition, many studies have shown that when HIV is undetectable, it is not transmissible4. Treatment is therefore also a prevention tool.

The best way to fight an infectious agent is to avoid catching it. This means identifying situations where there is a risk of transmission and taking precautions to avoid them (such as using condoms during sex). However, zero risk rarely exists and, for the past ten years, a new preventive tool has been available for people who do not feel sufficiently protected against HIV, whatever the reason: pre-exposure prophylaxis, or PreP. This approach consists of taking a combination of antiretrovirals before risky situations for uninfected people. Numerous trials have shown that this drastically reduces the risk of contamination, and studies are underway to evaluate different methods of administration (continuous or on-demand, oral or injectable, etc.), including one in the Paris region5. Despite its effectiveness, PreP is still not well known to the general public, but it is available in France from the age of 15 and is reimbursed by the French social security system.
HIV today
An estimated 190,000 people are living with HIV in France. This number is constantly increasing, as there are more new diagnoses than deaths of people with the virus every year. While the effectiveness of treatments is excellent news, the number of new infections has been relatively stable for the past ten years. It has decreased in 2020 and 2021, although it is not really possible to draw any conclusions, as the SARS-CoV‑2 health crisis has had complex repercussions on behaviour and the health system. In any case, it is estimated that around 5,000 people discovered their HIV status in France in 2021, 51% of whom linked their infection to heterosexual intercourse. Unfortunately, about 30% of patients were already at an advanced stage of the disease at the time of their diagnosis, a figure that has also been stable for the last ten years6.
According to UNAIDS figures7, globally, about 1.5 million people were infected with HIV in 2021 and 650,000 died of AIDS. An estimated 40 million people have died since the pandemic began in the 1980s, roughly the same number as are currently living with the virus. 15% of these people, or about 6 million, do not know they are infected, and a quarter do not have access to antiretroviral therapy. But these figures hide wide variations across the world.
Outside sub-Saharan Africa, 94% of new HIV infections are among sex workers, men who have sex with men, injecting drug users, transgender women, or the sexual partners of all of these. In sub-Saharan Africa, where the majority of HIV carriers live, only half of all new infections are among these groups. And 63% of those infected in 2021 were women or girls.
International targets are regularly set to try to end the HIV pandemic. The 2020 target has unfortunately not been met8 and the 2030 target can be summarised in three numbers: 95–95-95. That 95% of people living with HIV know their status, that 95% of those who know their status are on treatment and that 95% of those on treatment have an undetectable viral load9. In 2021, these figures were 85%, 88% and 92% respectively.
The fight against discrimination is also essential, as people with HIV suffer from strong serophobia, both in the medical environment, at work and in their private lives10. In a survey carried out in France in 2021, 36% of parents expressed discomfort at the idea of an HIV-positive person looking after their child11, even though this situation does not present any risk of contamination (which is non-existent in any case when treatment makes the virus undetectable). Education is therefore essential on these subjects.
Progress in HIV treatment and prevention approaches is to be celebrated, but the road to eradication is still long. Especially as we still have neither an effective vaccine nor a treatment that can cure the virus once and for all (although a few exceptional cases are known, to which we will devote a future article). Finally, let us salute the indispensable work of the associations which, since the beginning of this pandemic forty years ago, have played a fundamental role in prevention, support for patients and the fight against their stigmatisation.















