Algorithms, a major tool in the quest for “ageing well”
- Since the 1960s, human life expectancy has increased rapidly, but the years gained do not always go hand in hand with a “good quality of life”.
- At the same time as this demographic transition, climate change will have an impact on the human population, which will become more fragile with age.
- “Good health” is defined by the maintenance of functional capacities, i.e. a suitable living environment combined with good intrinsic capacities.
- Digital programmes such as ICOPE aim to prevent dependency among the elderly and ensure that they enjoy a good quality of life.
- These digital medical tools provide a personalised, patient-centred care pathway.
Life expectancy is increasing rapidly. Between the 1960s and the beginning of the 21st Century, the average lifespan has increased by around 20 years. However, these extra years do not always mean a “good quality of life”. Even though “geroscience” and medical progress are making it easier to understand the signs of ageing, the challenge today is to “age well”. To achieve this, the use of digital technology is a real opportunity. Algorithms, already used to prevent the onset of cancer or to predict epidemic risks, can now help anticipate dependency and age-related pathologies.
Digital medicine: an innovative program
The ICOPE (Integrated Care for Older People) digital programme, devised by the WHO, has been in use in France since 2019. For the first time, an experimental system is testing a new preventive approach, targeting the intrinsic capacity of patients over the age of 60. By self-assessment, or accompanied by a professional or non-professional carer, simple tests are used to assess six essential areas in the quest for a good quality of life:
- Mobility
- Nutritional status
- Mental health
- Cognition
- Hearing
- Vision
If any of these areas are found to be limited, the trained medical staff will carry out a more detailed clinical assessment and, if necessary, draw up a personalised long-term care plan. The care offered is varied (social support, home adaptations, physiotherapy, therapeutic adaptations, etc.) and depends on the pathology.
ICOPE, which originated in the Occitanie region of France, is now being rolled out nationwide. Today, 42,000 senior citizens are testing the programme, which will eventually enable benchmark standards to be set for age-related pathologies. The programme is available in the form of an application (ICOPE MONITOR) and a conversational robot (ICOPE BOT). Thanks to this, autonomous elderly people living at home are actively involved in strengthening or preserving their intrinsic capacities. At the same time, almost 10,000 healthcare professionals have been trained to respond to alerts.
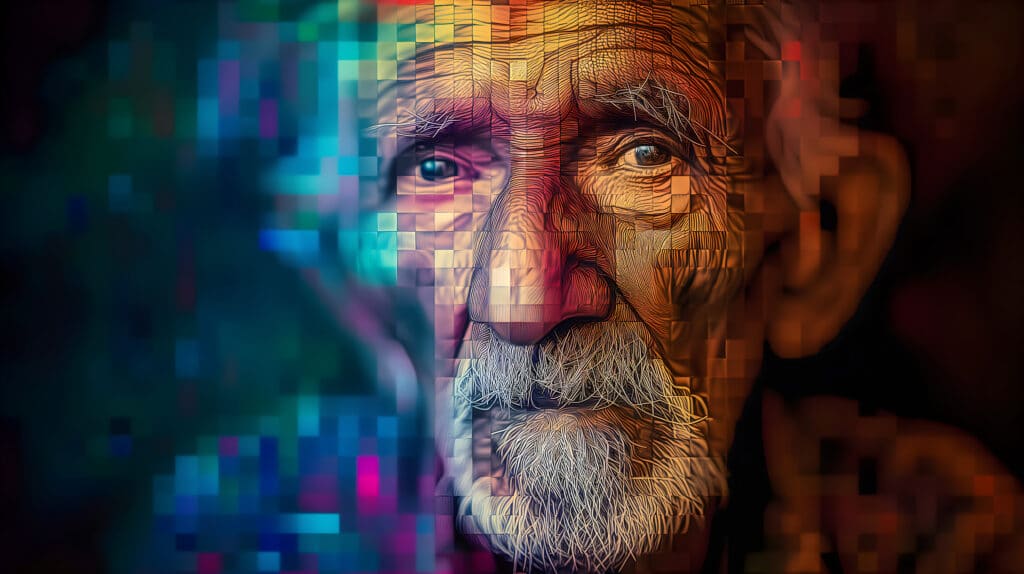
With this system being deployed over the last five years, the WHO is changing the definition of good health. Being in good health means above all maintaining good functional capacity. This is the result of a suitable living environment combined with intrinsic capacities, i.e. the maintenance of sensory, psychological, nutritional, motor and cognitive abilities. According to geriatric experts, these parameters have a major influence on healthy ageing. Preserving them delays the onset of dependency and therefore helps maintain a good quality of life.
ICOPE is an adaptive programme. It continues to be adjusted and deployed according to theoretical and practical observations. So far, this programme has proved that digital medicine can identify the determinants of frailty at an early stage, enabling early intervention with an integrated, personalised care pathway.
From managing dependency to preventing it
Compared with other forms of medicine, geriatric medicine has its own unique approach. While we usually look for a single pathology, in the field of geriatrics a variety of symptoms often arise from multiple factors associated with age (isolation, depression, malnutrition, etc.). The aim of this innovative digital tool is to put the patient back at the heart of the care pathway. We are no longer just treating illnesses, but the patient as a whole.
From observation to innovation
It was in the 1980s that Dr Laurence Z. Rubenstein was the driving force behind this idea. Seeing his patients seeking further consultations shortly after being treated, he suspected a flaw in the healthcare system. In 1984, he published the promising results of his study in the New England Journal of Medicine. The implementation of a global assessment of his patients, whatever the pathology that brought them in, made it possible to prevent their functional decline and preserve their autonomy. This project (carried out on a sample of 200 elderly people) was confirmed 10 years later by an initial meta-analysis. Gradually, there was a collective realisation that our healthcare system was not adapted to the needs of the elderly, who required comprehensive, individualised care.
Around 10% of seniors lose their independence during hospitalisation. To ensure a quality end to life, treating illness is not enough. By integrating digital medicine into care pathways (via systems such as ICOPE), the WHO has a number of objectives: to reduce the number and cost of hospital admissions, delay admissions to retirement homes and prevent functional decline.
The simultaneous threat of two major transitions
“We need to take a more global approach to the issue of the elderly”, says Yves Rolland. The world’s population is ageing rapidly. According to the WHO, the number of people aged 80 or over is set to triple by 2050. This demographic transition promises to dramatically change the world on numerous levels, starting with the healthcare sector. At the same time as the needs of an ageing population increase, the number of carers promises to fall sharply over the next twenty years or so. Added to this is an environmental threat. Climate change, which is already well underway, will have a major impact on a human population weakened by age.
This combination of threats makes preventive healthcare vital. It is crucial to reorganise the healthcare system, make it more accessible and step up our efforts in preventive communication. These efforts should not be confined to the hospital sector but should extend to the more “academic” disciplines. We’re talking about “health-bio-clinical-social-environmental” prevention. To put it plainly, ensuring “ageing well” requires maintaining health and independence through a variety of disciplines: meditation, sport, diet, psychology, etc. The aim is to reach a wide range of people, especially those furthest from the healthcare system.