It is clear that to avoid a health catastrophe, we must not only find new antimicrobial solutions but also reduce the unnecessary use of treatments; both complementary and vital solutions, according to the experts. And yet, when we look at the figures, the efforts are not yet highly noticeable.
Use may still be on the rise
Global consumption of antibiotics in hospitals between 2019 and 2020 according to Santé publique France rose by +2.1%. Even though, at the same time, consumption in towns and cities has decreased, largely due to the reduction in care caused by Covid lockdowns.
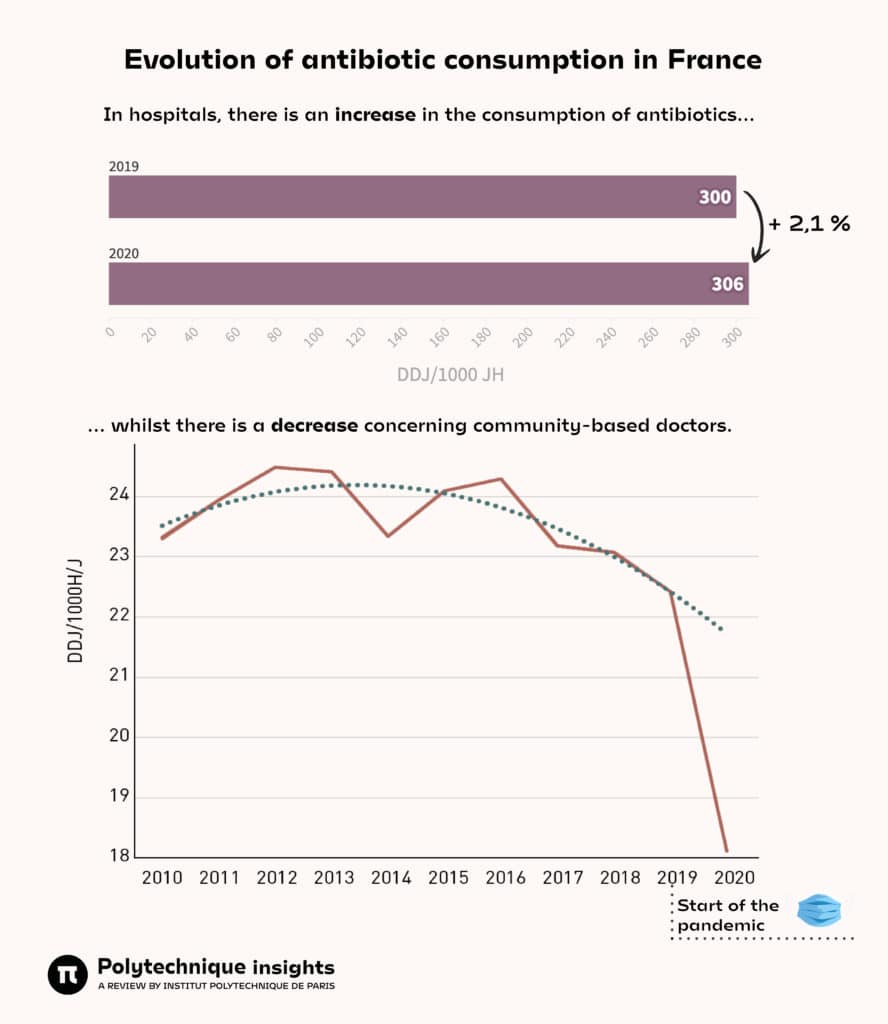
DDJ/1000H/J = Number of daily doses per 1,000 inhabitants per day.
Sources: Santé publique France, report in the hospital sector and in the community sector.
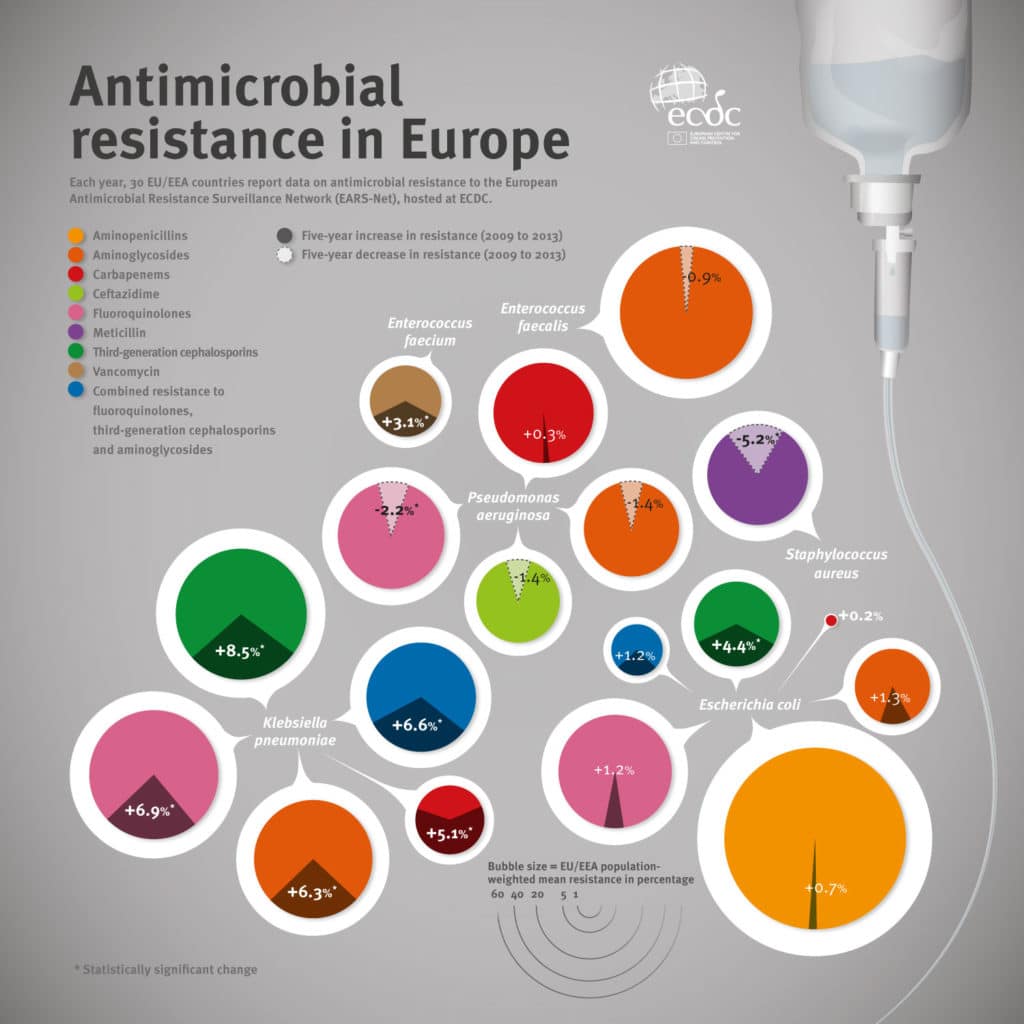
Data from the European Centre for Disease Surveillance (ECDC) show that even in Europe, resistance to treatment is present. For Klebsiella pneumoniae, most strains circulating on our continent are resistant to carbapenems, a widely used class of antibiotics. This trend is still on the rise despite the efforts of expert centres. On the other hand, meticillin-resistant Staphylococcus aureus is becoming less frequent. Progress is therefore possible.
And this trend is not limited to common antibiotics. This interactive infographic from the ECDC shows the growth of resistance against antibiotics of choice.
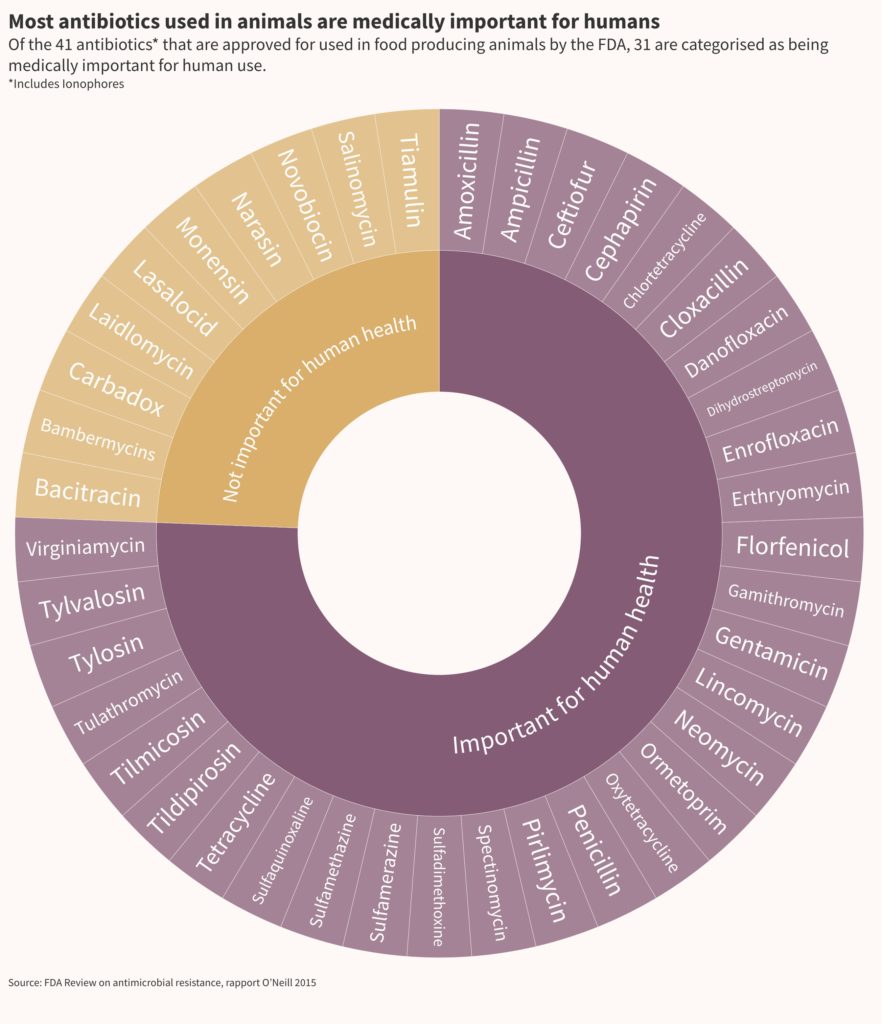
Agriculture is part of the problem
A human health issue, but also a veterinary health issue. The use of antibiotics in livestock is one of the driving forces behind the development of antimicrobial resistance. Although highly controlled in European farms, they are still generously administered to livestock in other regions. In the United States, this practice that promotes the growth of animals remains authorised but limited since 2017 to antibiotics that are not important for human health. But they remain appropriate for treatment and even remain the mainstay of the veterinary pharmacopoeia.
Solutions that are difficult to come by
50 new antibiotics are in development according to the WHO. 32 target pathogens considered to be a priority for human health, but the transnational medical authority recognises their limited benefit compared to existing molecules. Only two of them act on multi-drug resistant Gram-negative bacteria, strains whose health consequences are growing rapidly.
Most of these drug candidates are still in the early stages of evaluation and 252 antibiotic agents targeting priority pathogens are in pre-clinical phase. The small proportion of these molecules that will prove safe and effective in human health will not be available for another decade.